How to treat and help prevent IAD.

Incontinence-associated dermatitis (IAD) represents a significant health challenge worldwide. IAD can cause immense pain and discomfort for patients who are affected, and it can be difficult, time-consuming, and expensive for clinicians to treat.1
Also known as perineal dermatitis, or diaper rash, IAD refers to the irritation and damage that can occur after prolonged skin exposure to urine and/or feces. This can cause the skin to become inflamed and infected, which is why it is important to regularly assess risk factors and to recognize, categorize, and treat IAD accordingly.
Who is at risk for developing incontinence-associated dermatitis?
While IAD can affect any patient with urinary or fecal incontinence, patients with the latter are at higher risk of developing IAD than those with urinary incontinence alone.2
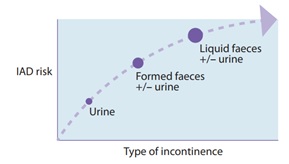
However, all patients who experience incontinence may be at risk of developing IAD, making it important to create individualized prevention plans to help reduce the risk of IAD and other associated conditions.
How to recognize and categorize IAD.
IAD initially appears as erythema, which makes the skin look pink to red (for light skin tones) or dark red to purple (for deep skin tones). Erythema may develop into the loss of skin thickness, resulting in excoriated, open, and weepy skin. Patients can experience pain and discomfort, such as burning, itching, or tingling in the affected areas.
Depending on the extent of contact with urine and faeces, IAD may affect large areas of the skin from the perineal region to the genitals, and even the abdomen and the anterior and medial thighs.
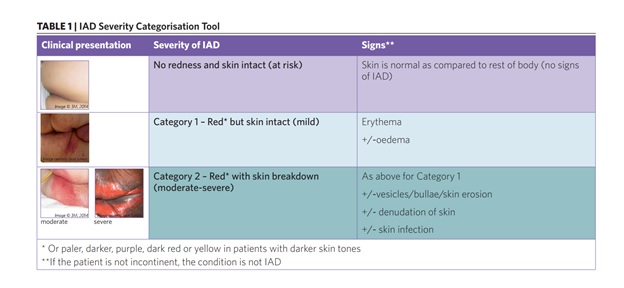
Graphic Image - Click to Reveal
How to prevent and manage IAD.
Treatment for IAD should focus first and foremost on the comprehensive assessment and treatment of the patient’s incontinence. This can involve non-invasive behavioural interventions, such as nutritional management, fluid management or toileting techniques.3
Once these interventions are undertaken, implementing a structured skin care regimen is paramount for the prevention and treatment of IAD. The aim of this regimen should be to:
- Cleanse: A skin cleanser with a pH range that is similar to normal skin is preferable to traditional soap.4 3M™ Cavilon™ No-Rinse Skin Cleanser dries quickly and can remain on the skin without irritating it.
- Protect: Skin protectants, like barrier creams, form a barrier between the skin and any additional moisture or irritants such as urine, faeces and/or friction.5 Depending on the severity of the wounds, 3M™ Cavilon™ Durable Barrier Cream, 3M™ Cavilon™ Moisture Barrier Ointment, or 3M™ Cavilon™ Advanced Skin Protectant can help prevent and treat this condition.
- Restore: As the skin heals, a barrier film, like 3M™ Cavilon™ No Sting Barrier Film, can help support and maintain the integrity of the skin barrier without causing pain or stinging.
Adding these three steps to a patient’s skin care regimen can go a long way toward managing and preventing IAD.
REFERENCES
- Doughty, D., Junkin, J., Kurz, P. et al. 2012. Incontinence-associated dermatitis. Consensus statements, evidence-based guidelines for prevention and treatment, current challenges. J WOCN 39(3): 303-15.
- Campbell, J. L., Coyer F. M., Osborne, S.R. 2014. Incontinence-associated dermatitis: a cross-sectional prevalence study in the Australian acute care hospital setting. Int Wound J. doi:10.1111/iwj.12322.
- Gray M. 2014. Incontinence associated dermatitis in the elderly patient: Assessment, prevention and management. J Geriatric Care Med.
- Beeckman, D., Verhaeghe, S., Defloor, T., et al. 2011. A 3-in-1 perineal care washcloth impregnated with dimethicone 3% versus water and pH neutral soap to prevent and treat incontinence-associated dermatitis. J WOCN 38(6): 627-34.
- Beeckman, D. et al. 2015. Proceedings of the Global IAD Expert Panel. Incontinence associated dermatitis: moving prevention forward. Wounds International. Available to download from www.woundsinternational.com.